By Santa J. Bartholomew M.D. FAAP, FCCM
As we head into fall with leaves falling and more rain, mold counts rise and there is a spike in winter viral infections. During this time, children with asthma come to emergency departments and get admitted to hospitals in droves.
Asthma is defined by episodic and reversible airway constriction and inflammation is triggered by many allergens. Among the top allergens are mold and viral inflammation, making fall and winter challenging for families of children with asthma. Because asthma is so common, affecting 1 in 12 American children and costing $80 billion/annum in medical care, not to mention missed school and missed work for parents, it has long been a disease that garners great interest in the prevention of episodes.
Drugs that provide relief during wheezing attacks still do not provide 100% of prevention from asthma attacks causing hospitalization. Further, asthma disproportionately affects minorities and socioeconomically disadvantaged children. Black children have the highest morbidity and mortality rates in the country and are 9 times more likely to die from their asthma than their white counterparts.
Pathophysiology of Asthma
Asthma exacerbations are the leading cause of ED visits and account for one of the top 3 reasons for admissions of children. The pathophysiology of asthma is a highly complex, immune-mediated inflammatory disease that causes intermittent and reversible lower airway obstruction which includes constriction of the smooth muscle of the airway and narrowing in the airway because of this constriction as well as mucous production caused by the triggering agent.
Asthma in children is so common, affecting 1 in 12 American children and costing $80 billion/annum in medical care…
The combination of these issues causes an obstructive pattern of breathing in which a child can inhale but cannot exhale the breath easily and over time this causes the lungs to over-inflate. This overinflation causes a feeling of shortness of breath and can actually impact blood flow in and out of the heart in severe attacks. The current understanding of asthma immunology suggests that the type and severity of asthma a child has may be related to exposures they have very early in life.
Common triggers
- Viruses: particularly rhinovirus and Influenza A are associated with the largest spike in asthma attacks in the fall. Influenza A associated pediatric deaths between 2000-2016 found that 12% of these children suffered from severe asthma exacerbations
- Irritants: cigarette smoke (many parents will attest to smoking outside the home but smoke imbedded in clothing is as powerful a trigger as direct exposure), candles, incense, vapor from electronic cigarettes, wood fire particulates, air pollution
- Allergens: mold spores, cockroaches and cockroach detritus, rat dander, mice dander, dust mites and pet dander
- Weather: rapid changes in temperature and/or barometric pressure
- Medications: B-blockers, aspirin, NSAID
- Exercise Induced: rare and more commonly found in poorly controlled asthmatics
- Poor Mental Health of Care Provider: usually associated with poor control of child’s asthma
Environmental Triggers
Environmental triggers are a major contributor to health disparities in pediatric asthma and a thorough review of these can reduce a child’s risk of having a life-threatening asthma attack as much as 40%, for example just removing triggers from the environment such as pets and carpet that can catch dander and mites.
Recommendations for trigger removal
- Dust mites—provide mattress and pillow encasements, vacuum twice a week, consider removal of carpet in the bedroom if there are significant nighttime symptoms, remove any stuffed animals from the child’s bed or recommend machine washing of stuffed animals in hot water
- Mold spores—avoid humidifier use; remediate and water damage/mold in the home
- Pests—keep food out of the bedroom and in closed trash containers, exterminate if needed (preference of traps over sprays)
- Animal dander—consider removal of animal if that is an option or recommend special hypoallergenic breeds
Diagnosis
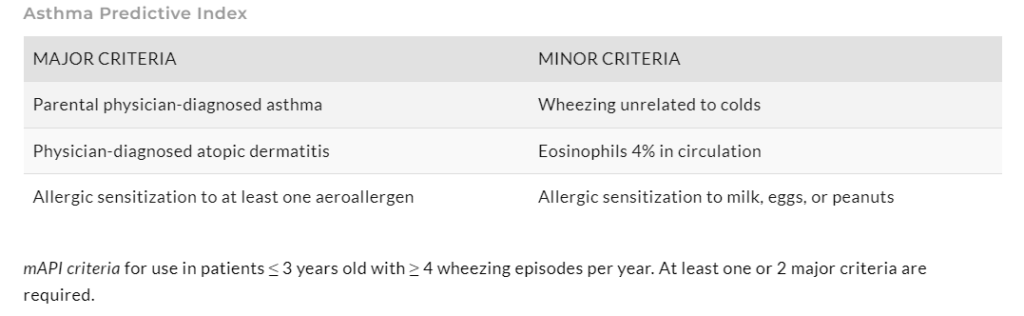
Diagnosis remains largely clinical as most children under 5 years old cannot perform the pulmonary functions tests (PFT’s) required for diagnosis. A child with a family history of asthma who has episodic and recurring chest tightness, cough and difficulty breathing +/-wheezing in response to common triggers most likely has asthma. These children may also have allergic rhinitis, eczema. There is now an Asthma Predictive Index to help outpatient providers objectively review symptoms to assist in diagnosis.
Of course, as a health care provider one must consider the other possibilities for wheezing other than asthma, which are many and age dependent including GERD, BPD, chronic aspiration, trachea and bronchomalacia, bronchiectasis, food allergy, panic attack, vocal cord dysfunction, foreign body aspiration, mass in airway or airway anomaly, cystic fibrosis. Once these are ruled out and the diagnosis of asthma is made then one can decide on a treatment path.
Treatment
The overall goal in treatment is to reduce impairment and maintain a good quality of life for the child allowing for exercise and play and keeping the child out of the hospital and off long-term systemic steroids if possible. Treatment is generally multi-pronged.
- Short term and acute treatment
- B-agonists like albuterol are the mainstay of treatment in exacerbations for quick relief of bronchospasm but may cause fast heart rate and shakiness.
- Anticholinergics
- Ipratropium bromide: takes longer to work than Albuterol but lasts longer so can be used in the ED together with Albuterol for short and longer term relief
- Steroids: short course
- Decadron, prednisone, or prednisolone in short courses can be used to abate inflammation in the airway but if used too often can cause adrenal suppression leading to catastrophic consequences.
- Controller medications to avoid exacerbations
- Leukotriene inhibitiors:
- Immunomodulators
- Inhaled steroids
- Long-term anticholinergics
- Inpatient adjunct medications
- Albuterol delivered in high doses via a continuous delivery system
- Large doses of IV steroid to quickly abate inflammatory response
- Magnesium sulfate
- IM epinephrine
- IV Terbutaline: IV B-agonist
- Helium
- General anesthesia
Conclusion
Asthma is a common problem in children and can be controlled with good control of environment and controller medications and aggressive attention to exacerbations. Most pediatricians are well educated in how to manipulate these medications for the best outcome, but this also relies on compliance of the family. Asthma is so common that people become complacent and stop taking their medications or expose themselves to risks like smoking which can lead to catastrophic consequences. Thousands of children die annually, unnecessarily, because of these actions.
In hospitals children die because they have been brought to medical attention too late, their bronchospasm cannot be broken quickly enough despite heroic activities. The best way to avoid these deaths is compulsive compliance to a medication and life plan.




