By Santa J. Bartholomew M.D. FAAP, FCCM
This case study discusses whether or not the patient is a candidate for procedural sedation.
John is a 16-year-old who presents for MRI of the head for persistent headaches and balance issues. He has been seen by neurology and there is concern for an anatomic brain issue. John, however, is profoundly afraid of enclosed spaces and has already tried and failed to do his MRI awake.
He presents to the sedation service with his dad for a pre-procedure evaluation approximately 4 hours before the procedure with the last 2 progress notes from his neurologist and the visit note from his PCP.
John is described as a healthy young man with no significant past medical history. He has exercise induced asthma uses his inhaler 3-4 times a year when playing sports but otherwise has not been hospitalized or in the ED for wheezing. There is no family history of anesthesia issues and John has never been sedated before.
Vitals: HR: 98 RR: 22 BP: 138/82 Weight: 261 pounds Height: 74 inches
The Physical Exam is remarkable for Mallampati 3 airway.
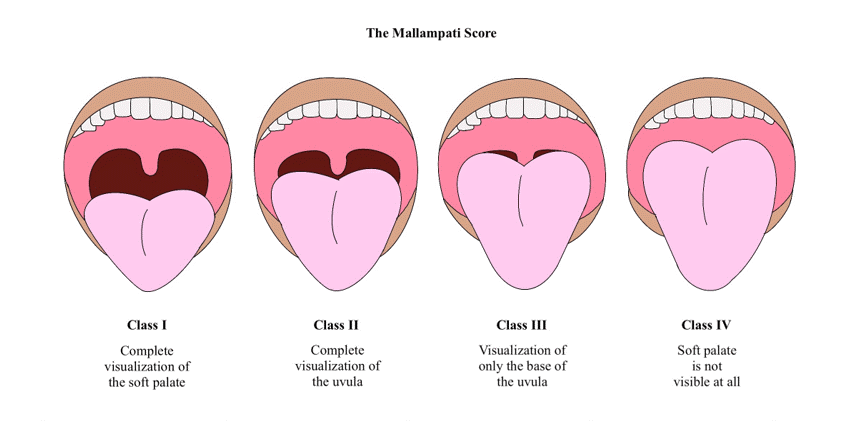
He can move his neck completely in all directions. He does not have a clear view of his tonsils. He has clear lungs. No murmur on auscultation of the heart. His abdomen is obese but soft and not tender.
After your physical examination you question John and his father about John’s sleep habits and find that John does not sleep in a bed but on a recliner because it helps with his “horrific snoring”. He has never had a sleep study because dad snores and he states: “Its just a hereditary thing”.
Do you proceed with this child’s out of the OR sedation?
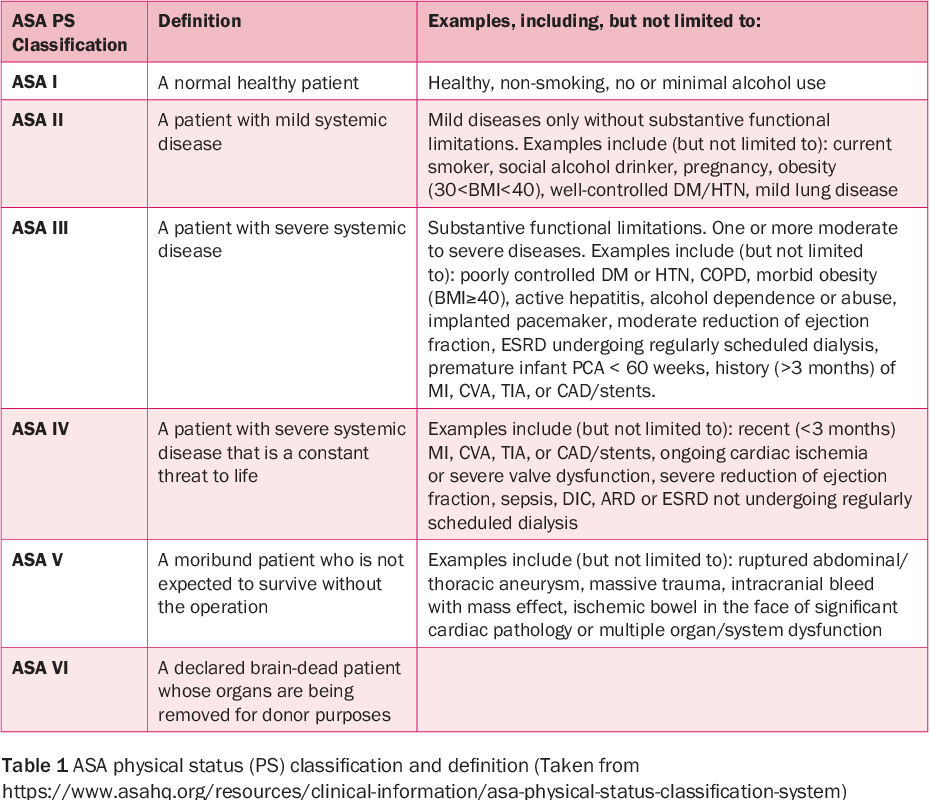
No, this child has what is considered a difficult airway: you cannot assess his entire throat because he cannot open his mouth wide enough, he has morbid obesity with a BMI 32.9, and snores suggesting sleep apnea. All of these issues make John an ASA 3 risk for sedation.
This means that he is more likely to have severe complications from sedation than another child who had none of these issues. You decline sedation and refer him to anesthesia for sedation.