By Santa J. Bartholomew M.D. FAAP, FCCM
The World Health Organization (WHO) has recently recommended “mpox” to be the new preferred term/synonym for Monkeypox. Both the Centers for Diseases control (CDC) and Health and Human Services (HHS) have adopted “mpox” as the new term used for Monkeypox.
Monkeypox is a virus belonging to the Orthopoxvirus genus in the Poxviridae family. Monkeypox primarily occurs in west and central Africa, often close to tropical rainforests. The first outbreak of Monkeypox outside of Africa occurred in 2003 in the United States. Since that time, Monkeypox has continued to be reported in several areas of the world including the United States.

A 7-year-old Zairian girl with monkeypox in the acute stage, day 7 of rash, and monkeypox in a 3-year-old Zairian boy with rash in the scabbing stage, DRC, 1970-1977. WHO / Mark V. Szczeniowski.
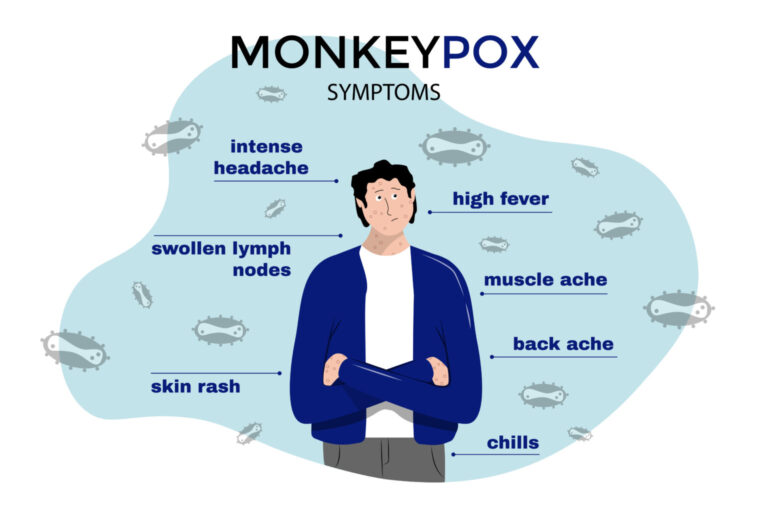
Signs And Symptoms of Monkeypox
Symptoms of Monkeypox are similar to those of smallpox, but often less severe. The time from infection to the onset of symptoms (Incubation period) can range from 5 to 21 days, but is usually 6 to 13 days.
Two Phases of Infection
- The Invasion Period: Lasts 0-5 days. Characterized by intense headaches, fever, swelling of the lymph nodes, muscle aches, back pain, extreme fatigue. Swelling of the lymph nodes is a primary feature of monkey pox not generally seen with other similar illnesses such as chickenpox, smallpox, and measles.
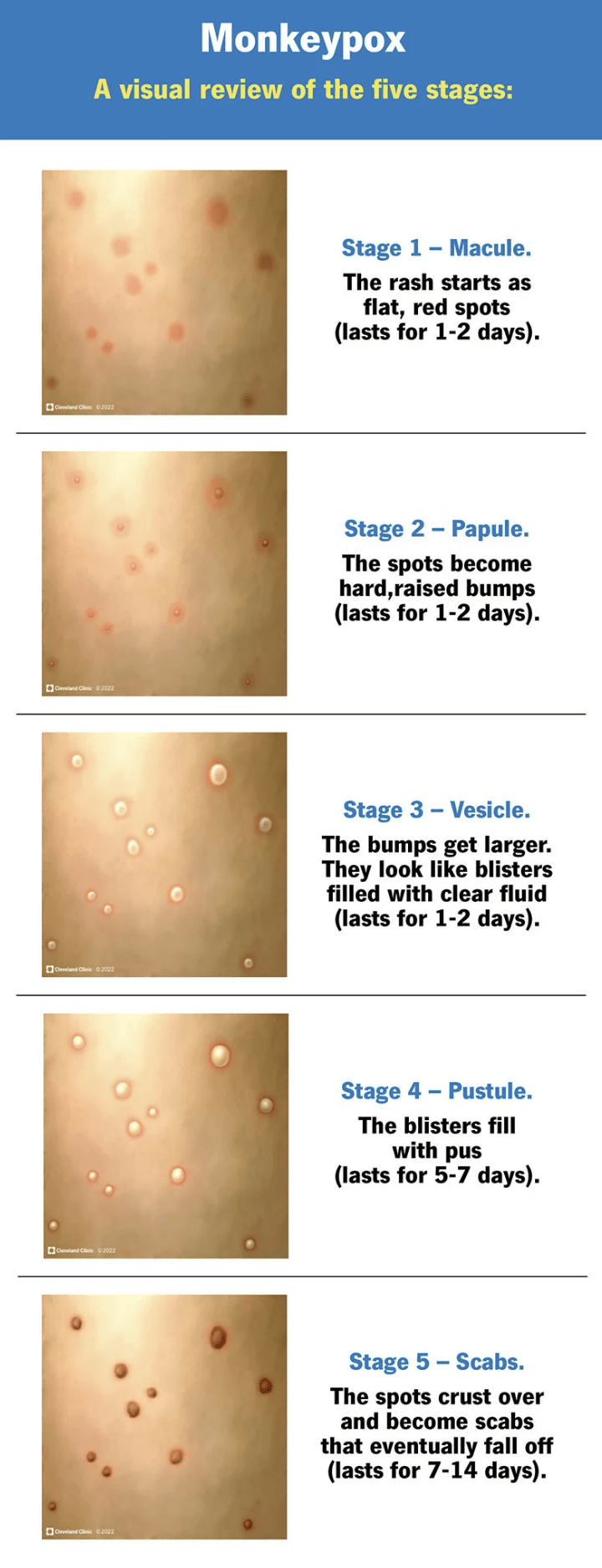
- The Skin Eruption Period: Usually appears 1-3 days following fever. The rash is usually seen more on the face, arms and legs rather than the trunk. Affects the face (95% of cases), palms of hands and soles of feet (75% of cases), oral mucous membranes (70% of cases), genitalia (30% of cases), conjunctivae (20% of cases) and cornea. The rash starts as flat lesions progressing to raised, firm lesions. These lesions then become filled with a yellowish fluid which then dry up and fall off. The number of lesions may vary from a few to thousands.
Monkeypox is a self-limiting disease. Symptoms generally lasts 2-4 weeks. Severe cases are more common in children. Severity of the illness is related to the extent of the exposure to the virus.
Complications of Monkeypox
Secondary infections, pneumonia, overwhelming infection/sepsis, encephalitis, infection of the cornea leading to vision loss.
How Is Monkeypox Transmitted
Transmission may occur from the mother to fetus via the placenta. This can lead to congenital monkeypox. Transmission may also occur due to close contact during and after birth. The risk of children and adolescents being infected with the monkeypox virus is low. Infants, children and adolescents may be at an increased risk of contracting Monkeypox if they suffer from eczema, other skin conditions, or immunocompromising illnesses.
Various animals have been identified as being susceptible to the monkeypox virus and therefore, becoming hosts for the disease. Animals included are rope squirrels, tree squirrels, Gambian pouched rats, dormice, non-human primates and several other species.
Transmission from animal-to-human may occur through direct contact with blood, body fluids, or skin or mucosal lesions of infected animals. Possible risk factors include eating meat that has not been cooked adequately and other animal products of infected animals.
Human-to-human transmission may also occur. This can result from close contact with respiratory secretions, lesions of the skin of an infected person, or touching recently contaminated objects. Transmission via respiratory droplets requires a prolonged length of time having face-to-face contact. This places health care workers, family members and other close contacts of active cases at an increased risk.
Diagnosis and Treatment
It is important to consider other similar illness when diagnosing:
- Other rash illnesses (chickenpox, measles, bacterial skin infections, scabies, syphilis, allergies from medications)
Diagnosis by PCR is the preferred laboratory test. Fluid from the vesicles/pustules and dry crusts. Biopsy may also be taken. PCR blood test often inconclusive. Previous vaccination with smallpox vaccine or monkeypox vaccine may result in false positive results.
Treatment includes
- Alleviating symptoms, managing complications and preventing long-term sequelae.
- Fluids and food are important to maintain good nutritional status.
- Secondary bacterial infections will also need to be treated.
- An antiviral (tecovirimat) was developed for smallpox and licensed by the European Medicines Agency (EMA) for monkeypox in 2022. This was based on data from animal and human studies. Not yet widely available
Prognosis
In the past, fatality ranged 0-11% (higher among young children). More recently, 3-6%.

Vaccination
Smallpox was eradicated in 1980 and there was subsequent cessation of the smallpox vaccine. Being vaccinated against smallpox has been shown to be approximately 85% effective in preventing monkeypox. Due to no longer manufacturing the smallpox vaccine, persons under 40 to 50 years of age may be more susceptible to monkeypox.
A newer vaccine was approved in 2019 for the prevention of monkeypox. This is a two dose vaccine, but availability is limited.
Prevention
- Be aware of risk factors
- Educating about measures to reduce exposure to the virus is the key to prevention
- Possibility of more widely available vaccines in the future
References:
Monkeypox. (n.d.). https://www.aap.org
Mpox. (2022, December 8). https://www.cdc.gov
Monkeypox. (2022, May 19). https://www.who.int




