See Corresponding Case Study: Pediatric Diabetic Ketoacidosis
Many people in the United States have diabetes mostly secondary to the preponderance of obesity in our nation and the general lack of exercise.
We are seeing more and more young people, as well as the elderly, with Type 2 diabetes which is a resistance to insulin that is made by the pancreas. This resistance develops over time from diets that include large amounts of simple sugars and carbohydrates and not enough vegetables or protein. Each time there is a large carbohydrate meal the body secretes insulin that in turn allows the body to use this meal as energy.
Unfortunately, simple carbohydrates, like cakes, snack foods, French fries and the like are quickly converted to sugar and cause large spikes in insulin and are quickly gone from our system creating hunger again and making us crave more carbohydrates. This cycle repeats itself over and over causing many insulin spikes per day and eventually the body reacts to this overload of insulin by taking away some of the receptors on the cells for insulin. This makes one even more resistant to insulin. Type 2 diabetes rarely results in very high levels of acid in the blood or extremely high sugars because in these individuals there is no lack of insulin just too much carbohydrate exposure.
Type 1 Diabetes
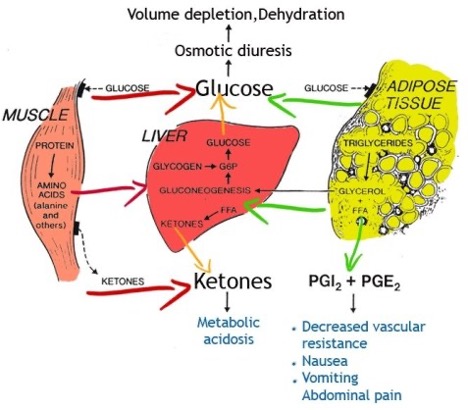
Type 1 diabetes is often diagnosed in childhood and is secondary to a failure of the pancreas in the affected individual to make insulin. There are a variety of reasons why this happens but the lack of insulin is the final common pathway. Without insulin, the carbohydrates that we eat cannot be metabolized to useful energy in our bodies and the simple sugar circulates in the bloodstream with no way to be utilized.
Type 2 diabetes rarely results in very high levels of acid in the blood or extremely high sugars because in these individuals there is no lack of insulin, just too much carbohydrate exposure.
The body is starving because it cannot use the substances we have eaten and so it changes its metabolism to use fats and glycogen stored in the liver and available in the body. The use of these alternate sources of energy cause the buildup of byproducts known as ketones as well as acid that then begins to circulate in the blood along with the circulating sugar. When the ketones and sugar get high enough in the bloodstream, they begin to spill into the urine.
As these excessive amounts of sugar spill into the urine the child begins to make vast amounts of urine as water is pulled towards the sugar molecules and is urinated out with the sugar into the urine. The child becomes profoundly thirsty and begins to drink enormous amounts of water and other liquids. If these are sugar-containing drinks, like sports drinks, the problem becomes worse and worse as the sugar in these drinks worsens the problem. At the same time acid from the use of fat for energy is also pouring into the blood making the child work harder to keep balance in the blood; this is seen clinically in the child breathing rapidly and deeply (Kussmaul breathing). Children may also experience vomiting and abdominal pain from the acid build up in blood and this usually leads to a doctor visit and diagnosis.
Dehydration
During this process that can last 2-3 weeks, the child becomes increasingly dehydrated as they cannot keep up with their urine losses and they lose weight in significant amounts because the body does not have the correct hormones (insulin) to make food into energy. As this process is occurring the body takes several actions to protect the brain from dehydration but if the child does not get to medical attention soon enough, even these actions are not enough and they begin to become lethargic as the brain becomes poisoned by the circulating ketones and acid.
Common Errors
When the child finally gets to medical attention this is usually via an emergency department that may not be skilled at caring for Type 1 diabetes and there are several common errors that occur as adult care providers use their knowledge of type 2 diabetes and apply it to these critically ill children.
- Because the child’s blood sugars are usually very elevated they are given a bolus of insulin. However rapid decreases in blood sugar in children in DKA can cause abrupt shifts in fluid in the brain and cause brain herniation.
- They are given too much IV fluid resuscitation and this fluid causes rapid swelling of brain cells and can cause death from herniation of the brain.
- They are given IV sodium bicarbonate to adjust the blood pH but this makes the brain cell ph (inside the cell) worse and can cause brain injury.
Although, all these actions may be exactly how to care for a sick adult with hyperglycemia and type 2 diabetes they are all contraindicated in the care of children and can accelerate their death from brain injury.
Reversing DKA
Reversing DKA requires a slow and measured approach in an intensive care unit specifically for children. Insulin is slowly introduced back into the body in an IV as well as fluids and electrolytes (salts the child has lost in the urine over the previous weeks of illness). The acidosis in the blood is never treated with bicarbonate as it may injure the brain cells but instead is treated by turning off use of the metabolism of fats in the body by introducing insulin back into the body. All of the care of the critically ill diabetic child is focused on slow rehydration while protecting the brain. During this process children are not permitted to eat or drink so that all fluid entering the body is carefully monitored to prevent brain swelling; along with hourly monitoring or frequent attention to body salts and acid in blood as well as attention to the child’s wakefulness and neurologic status.




