By Santa J. Bartholomew M.D. FAAP, FCCM
See Corresponding Case Study: Persistent Pulmonary Hypertension
A baby in utero does not require oxygenation via its lungs; rather, it is oxygenated by maternal respiration and placental oxygen supply. The alveoli, or the “air sacks” in the lungs, are full of fluid because they are not used to oxygenate the blood. The alveoli still have blood vessels going past them as they prepare to sustain extrauterine life. Because of the lack of oxygen in utero, there is a phenomenon called hypoxic pulmonary vasoconstriction, which is the clamping down of the blood vessels. This process is a clamping-down of the blood vessels in response to the lower oxygen level in the fetus. The pressure or resistance is increased like a hose that is being stepped on. The high pressure inside the vessel makes the pressure in the pulmonary artery very high so that flow into the pulmonary artery is virtually obstructed. This causes higher back pressure in the right ventricle and atrium.
Blood flow from the placenta then bypasses the infants’ lungs because of this high pressure is shunted to the baby’s body via two mechanisms: the foramen ovale (a hole in between the right and left upper chambers or atria of the heart) and via a bypass vessel between the pulmonary artery and aorta called the patent ductus arteriosus (PDA). These structures are unique to newborns.
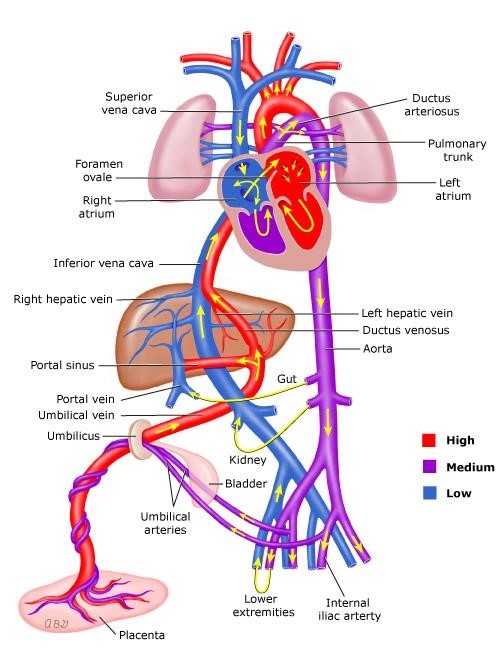
Persistent pulmonary hypertension of the newborn (PPHN) occurs when this pulmonary vascular resistance (PVR) remains abnormally high after the baby is delivered, causing shunting of blood through fetal circulatory pathways that should otherwise have closed shortly after birth.
Persistent pulmonary hypertension of the neonate (PPHN) is the failure of the normal circulation to transition to that which occurs after birth and is sustained for the rest of the life of the infant. It is a syndrome characterized by marked elevated pressure in the lungs due to persistent clamping down of the blood vessels and abnormal blood shunting at the foramen ovale and ductus arteriosus.
A series of diagnostic tests should be done to determine if the newborn has PPHN and the cause of the PPHN but ECHO is the gold standard way to determine the pulmonary pressures in the heart and make the diagnosis of PPHN. PPHN can occur when an infant has aspiration of meconium during the birth process, or blood or amniotic fluid, or some other irritant causing respiratory distress. It can occur from aspiration of any substance that injures the surfactant (a chemical in the alveolus of the lung that decreases surface tension and allows the lung to inflate) in the lung. It can occur from overwhelming infection in the infant.
Finally, the severity of the PPHN should be assessed. The best way to do this is to measure the oxygen index, a calculation where the provider multiplies [MAP x FiO2 ÷ PaO2] x 100. A severity quotient will be determined. With that, the provider can predict whether the baby will do well without much support, with a short period of support, or a baby who may need extra corporal membranous oxygenation or ECMO.
Treatments:
- Oxygen: usually delivered via high-flow nasal cannula (HFNC) at 100% or in severely distressed infants they may require mechanical ventilation.
a. Oxygen is an effective vasodilator, so the hope is that this treatment will decrease lung vasoconstriction. - Sedation: keeping the infant calm allows the pulmonary pressures to fall and in mechanically ventilated infants they may be chemically sedated and paralyzed.
- Nitric Oxide: a gas that is a profound vasodilator and can be administered via the ventilator. If needed this can then be converted to an oral medication that increases the levels of nitric oxide in the infants lungs long term called Sildenafil.
- ECMO: the infant is placed on a machine that oxygenates blood outside the body while all the other therapies are continued until the pressures in the lungs begin to fall.
The morbidity and mortality associated with persistent pulmonary hypertension of the newborn are related to the severity and duration of low systemic oxygen. If it is not treated, many infants are profoundly brain injured or die.
Current treatments are often ineffective, and more invasive therapies, such as ECMO, cause life-threatening complications and sometimes death. For these reasons, a rapid-acting, easily administered agent that selectively dilates the pulmonary vasculature and increases systemic oxygenation is essential such as nitric oxide have been revolutionary in caring for these infants. Inhaled nitric oxide rapidly increased oxygenation in infants with severe hypoxemia and pulmonary artery hypertension without causing systemic hypotension. In addition, long-term therapy with inhaled nitric oxide caused lasting improvement in oxygenation and reduced the requirement for extracorporeal membrane oxygenation.
References:
Jobe AH, Kallapur SG. (2010) Long-term consequences of oxygen therapy in the neonatal period. Semin Fetal Neonatal Med. 15(4):230-5. doi: 10.1016/j.siny.2010.03.007.
Murthy, P. R., & AK, A. K. (2022). High-Frequency Ventilation. In Stat Pearls. Stat Pearls
Pedersen, J., Hedegaard, E.R., Simonsen, U., Krüger, M., Infanger, M. and Grimm, D. (2018),
Current and Future Treatments for Persistent Pulmonary Hypertension in the Newborn. Basic
Clin Pharmacol Toxicol, 123: 392-406. https://doi.org/10.1111/bcpt.13051
Roberts, J , Fineman, J, Morin, F, Shaul, P, Rimar, S, Schreiber, M, Polin, R, Zwass, M, Zayek,
M Gross, I, Heymann, M, Zapol, W, Thusu, K, Zellers, T., Wylam, M, Zaslavsky, A. (1997)
Inhaled Nitric Oxide and Persistent Pulmonary Hypertension of the Newborn. New England
Journal of Medicine. 336(9) 605-610 doi10.1056/NEJM199702273360902
Stark, A., Eichenwald, E. (2023). Persistent pulmonary hypertension of the newborn (PPHN):




