By Santa J. Bartholomew M.D. FAAP, FCCM
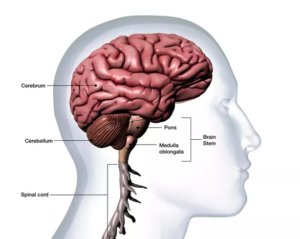
Ataxia is a word that derives from the Greek – ἁ (without), taktos (order). It means lack of order and encompasses disorders that involve uncoordinated motor movements involving walking or gait. This disorder of movements or ataxia in children most commonly comes from problems in the portion of the brain called the cerebellum but can also come from problems in the spinal cord or the nerves going to the muscles in areas far from the brain. Ataxia can be intermittent, chronic, subacute, or acute (less than 72 hours). In this article we will focus on acute ataxia and come back to other causes in the future.
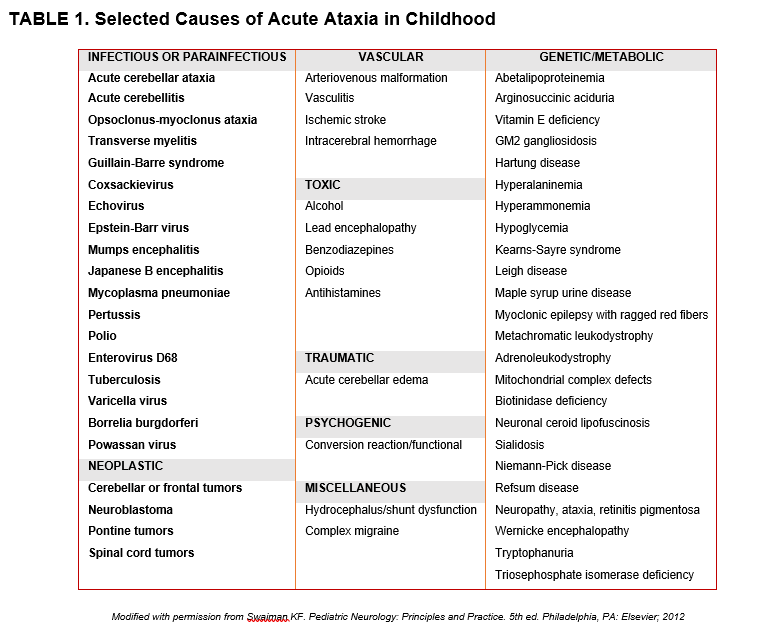
Life-threatening ataxia falls into 4 broad categories: infectious, vascular, toxic, or genetic/metabolic.
The healthcare provider must obtain a thorough detailed history and thorough examination as well as some laboratory and radiologic tests to assess if the ataxia is life-threatening. Life-threatening ataxia falls into 4 broad categories: infectious, vascular, toxic, or genetic/metabolic. Detailed history and physical examination will often direct the path of inquiry in assessing the cause of the illness. Questions about rashes, fever, respiratory or GI symptoms as well as trauma, use of medications prescribed or illicit as well as possible toxic exposures (such as lead) in the home all must be investigated to find the right course towards diagnosis of the etiology and subsequent treatment. Most acute ataxia is benign and self-limited but this extensive history and physical with some testing is needed to rule out life threatening disorders.
Acute cerebellar ataxia (ACA); the most common ataxia in children is characterized by the child maintaining alertness so ataxia associated with vomiting or change in mental status, headaches that wake them from sleep and vision issues is more likely brain tumor or increased intracranial pressure than it is benign ACA. Ataxia with only altered mental status can be infection, toxic ingestion or brain abscess or tumor so careful, meticulous history of the gait issue and associated problems is tantamount. Abrupt onset of symptoms is usually more likely infectious, toxic ingestion or vascular in nature whereas symptoms that occur over weeks to months are more suggestive of a chronic disease such as migraine vestibular issues, or metabolic disease or a slow-growing tumor or some kind of immune-mediated process.
Physical examination must include a complete set of vital signs including blood pressure as some diseases such as Guillain Barre Syndrome which can cause ataxia also have autonomic instability. Carefully look for evidence of neck stiffness, pain with light (photophobia), discomfort moving eyes around, any process which causes pain or swelling in the extremities or back that might suggest a “non-brain” cause of the ataxia such as foot problems, back spasm, scoliosis. Pupils can help suggest possible etiologies – such as large wide-open pupils occur with drugs like atropine and atropine like drugs and narcotics cause pinpoint pupils. Is there a droopiness to the eyelids which may suggest compression of the 3rd nerve that causes this symptom?
Neurologic examination is very important:
- Are there behavior changes in the child?
- Irritability
- Changes in alertness
- Abnormal patterns of speech
- Look in the back (fundus) of the eye looking for swelling which may suggest a brain swelling issue.
- Absence of venous pulsations around the optic nerve suggests increased intracranial pressure.
- Observe the child walk?
- Is the gait wide or narrow? Narrow gaits are unlikely to be ACA.
- IS the gait lurching or falling to one side? Typical of vestibular disease.
- Can the child stand with feet close together with eyes open and closed (if child falls or falters with eyes closed this is a + Romberg sign) suggests sensory ataxia. This occurs with issues of the spinal cord, vitamin deficiencies (B, Copper), alcohol intoxication.
- Are the reflexes normal, hyperreflexic or absent?
- Can the child sit up without support?
- Look for other signs of cerebellar dysfunction such as finger to nose dysmetria, palmar drift
- Weakness in arms? Bilateral or unilateral
Laboratory tests and radiology examinations:
- Urine toxicology
- White count with differential
- In some circumstance lumbar puncture may be warranted: ACA usually has a normal white count or mild elevation.
- CT/ MRI of brain if there is a focal neurologic exam and MRI of the spine in some cases.
What are you aiming for?
LOCALIZE THE REASON FOR THE ATAXIA AND THEN FIND THE REASON.
- Is it life threatening such as a stroke which is a medically emergency!!
- Most common cause in children is an intracranial hemorrhage from an arterio-venous malformation of blood vessels in the brain. CT and MRI are very useful in these circumstances and neurosurgical intervention absolutely necessary.
- Trauma: in the event of ataxia associated with a traumatic even this is also often a medical and surgical emergency portending arterial dissection and ischemia and although unusual in children it’s rapid recognition is key to meaningful survival
- Toxic ingestions account for approximately one third of children presenting to ED with ataxia. Urine drug screening (UDS) is very helpful in narrowing the possibilities and together with physical examination (looking for toxidromes: sets of symptoms that go with known toxins) can assist provider in treatment. When considering a toxin always make sure you check blood sugar, serum ammonia and serum sodium- these can all cause ataxia.
- Immune mediated/Post-Infectious (ACA, Cerebellitis, ADEM, GBS, Transverse Myelitis): child typically has had a viral infection in the past and now is presenting with ataxia. This is usually sub-acute presentation over a few days. Usually benign and self-limited.
- Typically occurs in preschool children
- Ataxia is most common on awakening and improves during the day.
- Truncal ataxia very common.
- Children are generally well appearing and afebrile although children with cerebellitis appear more ill than those with ACA.
- Patients with cerebellitis may have seizures, altered mental status and vomiting and this can become life threatening but is far less common than ACA.
- It is important to sort through the different immune mediated diseases as treatment types and length varies. These sub-acute causes of ataxia will be discussed in a future blog article
- Tumor: Childhood brain tumors most frequently in posterior fossa. Usually, the ataxia associated with these is slow to develop as the tumor obstructs CSF flow although there have been case reports of acute ataxia in these children.
- Migraine: vertigo can occur in very young children and teenage girls usually lasting second to minutes. Usually with a normal neurologic examination.
- Psychogenic Conversion Disorder: conversion reactions can range from unsteady gait , tripping and falling to a weaving and bobbing gait called atasia-abasia. This requires careful neurologic exam to rule out other causes that could be harmful to the child and then gentle confident communication of diagnosis with parent and child.
- Metabolic disease: very uncommon cause of ataxia. In young children metabolic disease can be discerned with a lactate and an ammonia and lead the examiner in the correct direction.
Treatment: is linked to cause of the ataxia but ACA the most common cause of ataxia in children is usually self-limited and benign requiring no medication for treatment. The key, however, as in many diseases is careful attention to the signs and symptoms and a correct diagnosis.