By Santa J. Bartholomew M.D. FAAP, FCCM
How Does This Happen?
Brain Abscess in children are very uncommon in both children and adults. A brain abscess is an infection pocket in the brain itself. They have become even more rare in recent years because of the better imaging techniques currently available. Overall brain abscess occurs in 1 per 100,000 people and about 25% of these cases are in children between four (4) and 10 years old with a small predilection towards boys.
Reduction in risk factors like sinusitis, middle ear infections, poor dental hygiene, un-repaired blue congenital heart disease, injuries with sharp objects (toys, pencils, chopsticks), immunosuppression (HIV, immunosuppression with organ transplant and hereditary diseases), and complications of brain surgery are the reason for the declining incidence of brain abscess; however, in children who do suffer from this infection the consequences of the disease are significant and the death rate equally as high.
The location of the brain abscess depends in general on the location of the primary (or original) abscess. The most frequent site is the frontal lobe of the brain as it is just below the frontal or ethmoid sinus and right near the upper teeth. Parietal or temporal abscesses are more common in chronic ear infections and sphenoid sinusitis. The lower part of the brain (cerebellum and brainstem) are infrequent locations usually seen with the spread of infection through the bloodstream. The infection in these primary sites breaks through the bony barrier to the brain causing infection within the brain. More rarely does the abscess form by bacteria traveling in the bloodstream to the brain.
Parietal or temporal abscesses are more common in chronic ear infections and sphenoid sinusitis.
Most common organisms
- 36%: Streptococcus
- 18% Staphylococcus
- 16% Gram Negative bacteria (Klebsiella, E.coli, Enterobacteria)
- Remaining: a mix of other bacteria and fungi
Symptoms
Symptoms are dependent upon the site and size of the abscess, the involvement of other areas of the brain and swelling surrounding the area of the abscess.
- Fever occurs in 30-70% of children – new onset headache typically associated with vomiting.
- Seizures occur in up to 70% of children with as many as 50% experiencing ongoing long-term seizures.
- Stroke-like symptoms such as hemiplegia, palsy of the cranial nerves, and altered consciousness.
- Infants may have bulging fontanelles.
Unfortunately, the clinical triad (as shown below) only occurs in a small group of children.
How do we find the abscess?
- Level of suspicion based on history.
- CT scan: 95-99% sensitive in spotting the lesion but hard to determine by CT if the lesion is an abscess, a tumor, or a vascular lesion.
- MRI: Better at demonstrating what the lesion is, can also give more information about swelling of the brain and look for smaller abscesses in the brain.
- High white count, sed rate, and CRP are found in most children with brain abscesses but are not specific to the disease.
Treatment
- Surgery to drain the abscess.
- Intravenous antibiotics.
- Repair of the underlying problem that caused the abscess.
- Treat side effects of abscess: brain swelling, seizures, bacteria in the blood.
Prognosis: 4-12% death rate
- Children that present with multiple abscesses or a very large deep abscess tend towards worse outcomes.
- Children with a rupture of the abscess into the intraventricular space have a worse outcome.
- 50% of children have ongoing seizures.
- Poorer intellectual outcomes in younger children.
- Delay in diagnosis also alters the long-term outcome.
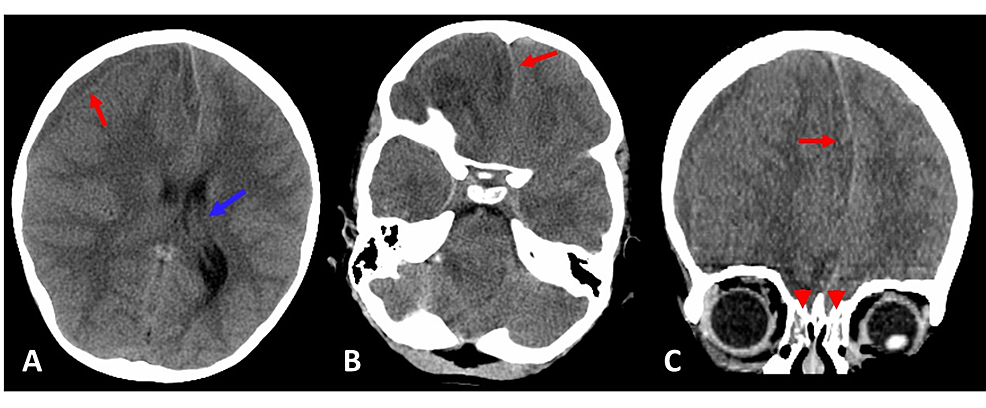
Figure 1: Computed tomography brain without contrast: hypodense right frontal temporal subdural hematoma extending along the anterior falx measuring 8 mm in greatest dimensions and causing right to left midline shift measuring 7 mm (red arrows). (A) Transverse view showing dilatation of the left lateral ventricle including the temporal horn concerning for mild entrapment (blue arrow). (B) More caudal transverse view showing midline shift (red arrow). (C) Coronal view showing midline shift (red arrow); there was also bilateral ethmoid sinusitis (red arrowheads).*




