By Santa J. Bartholomew M.D. FAAP, FCCM
An eight-year-old female presents to her Primary Care Provider (PCP) with a two-day history of fever, sore throat, nausea, and stomach ache. Upon exam, PCP visualizes pharyngeal erythema with white pustules and palate petechiae. Rapid strep test positive for streptococcus pyogenes group A (GAS).
The patient is prescribed Amoxicillin 25 mg/kg po every 12 hours for 10 days. Despite taking the Amoxicillin as prescribed, the patient continues to have fever, poor appetite, decreased fluid intake, and increased fatigue.
On day 7 of illness, the mother and father are having difficulty keeping the patient awake and her fever is 103.7 F (39.8 C). Upon arrival to the ED, the eight-year-old female is noted to be tachycardic with HR 138, experiencing rapid, shallow breathing, and hypotensive with BP 68/32. A widespread red flat rash is noted.
The medical team initiates fluid resuscitation, and IV antibiotics are started immediately following stat blood cultures being obtained. The patient’s blood pressure does not improve with fluid resuscitation and inotropes (medications to support her blood pressure) are started. A breathing tube is placed to support the child’s breathing.
Despite medications and fluid, the patient remains hypotensive (low blood pressure) with poor perfusion/blood flow to her extremities and body tissue. The medical team recognizes the child is in toxic shock syndrome and the child’s clinical status is rapidly deteriorating. The decision is made to deploy the Extracorporeal Membrane Oxygenation (ECMO) team and place the child on venoarterial (VA) ECMO.
What is Extracorporeal Membrane Oxygenation (ECMO)
Extracorporeal Membrane Oxygenation (ECMO) is a machine that works as the heart and lungs to support the body when the body and the organs are too sick to support themselves. Individuals may be on ECMO for a few days up to several weeks. ECMO allows the body time to rest and heal.
Types of ECMO
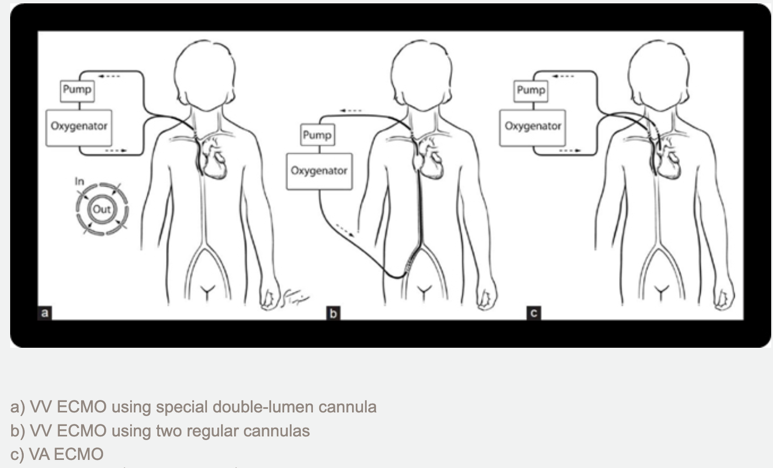
There are two types of ECMO: Venoarterial (VA) ECMO and Venovenous (VV) ECMO
Venoarterial (VA) ECMO: Provides support for the patient’s heart and lungs. A cannula is placed in a large vein and a large artery and connected to the ECMO circuit. Blood leaves the body through the cannula in the large vein, moves through the circuit where it is oxygenated by an oxygenator and returns to the body via the cannula in the large artery. This provides oxygen-rich blood to the body, and allows the heart and lungs to rest. The oxygenator additionally removes carbon dioxide from the blood.
Venovenous (VV) ECMO: Provides support and rest only to the lungs. The patient’s heart must still be strong enough and function well enough to meet the needs of the body. In VV-ECMO, one cannula with two lumens may be placed in a large vein close to or inside the heart, or two cannulas may be placed in veins close to or inside the heart. The cannulas allow blood to leave the body, move through the circuit where it is oxygenated by an oxygenator, and returns to the body before the heart, and the patient’s heart then pumps blood through the body. The oxygenator additionally removes carbon dioxide from the blood.
In this case study, the eight year old female developed toxic shock syndrome (TSS) following an infection with streptococcus pyogenes group A (GAS). The toxins (exotoxins) cause widespread inflammation to the body causing hypotension (low blood pressure), tachycardia (increased heart rate), faster breathing and organ failure. Venoarterial ECMO was initiated to take over the work of her heart and lungs and allow her body time to heal and rest.
“Types of ECMO | Extracorporeal Membrane Oxygenation | ECLS.” Www.elso.org, www.elso.org/ecmo-resources/types-of-ecmo.aspx.
Risks and Complications of ECMO
Although ECMO is a potential life-saving measure, there are several risks that may lead to morbidity and mortality. Risks include, but are not limited to, the following: bleeding, neurological events (i.e. seizures, stroke), vascular sequalae, blood clots, and infection.
Conclusion
ECMO is initiated when the heart and lungs , or just the lungs, need time to heal and rest. Medical situations that may be an indication for ECMO include, but are not limited to, following open-heart surgery, cardiac arrest, respiratory failure, and sepsis. In this case study, resuscitative measures including fluid boluses and medications to support her blood pressure were not meeting the demands of her body. Research indicates the use of ECMO in pediatric patients with sepsis and refractory shock is associated with survival rates up to 59%, with neonates having a higher survival rate.
References:
Ramanathan, Kollengode, et al. “Role of Extracorporeal Membrane Oxygenation in Children with Sepsis: A Systematic Review and Meta-Analysis.” Critical Care, vol. 24, no. 1, Dec. 2020, https://doi.org/10.1186/s13054-020-03418-z. Accessed 13 Jan. 2022.
“Types of ECMO | Extracorporeal Membrane Oxygenation | ECLS.” Www.elso.org, www.elso.org/ecmo-resources/types-of-ecmo.aspx.





