By Santa J. Bartholomew M.D. FAAP, FCCM
Mechanical ventilation is often required for critically ill patients in the ICU. As the acute phase of illness resolves, the goal is to wean the ventilator, allowing the patient to breathe more on their own (spontaneous breathing trials), and to successfully extubate, or remove the artificial airway. Patients may tolerate weaning the ventilator, but fail extubation. Extubation failure is defined as the inability to sustain spontaneous breathing after the removal of the artificial airway (an endotracheal tube or tracheostomy tube) and require reintubation within a specified time period, usually defined as 24-72 hours or up to 7 days.
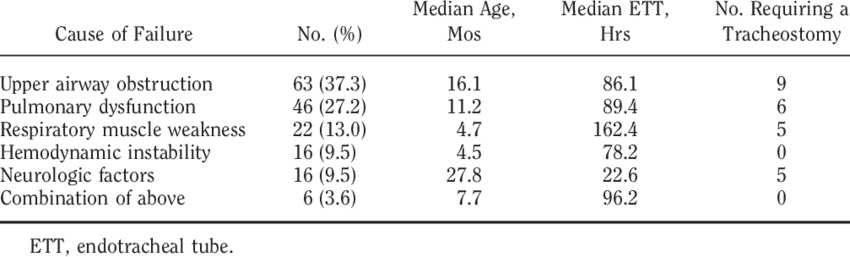
Causes of Extubation Failure
- Excessive secretions affecting airway patency
- Respiratory Failure: Most common cause. Manifest as increased work of breathing, hypoxia (insufficient oxygen), hypercapnea (excessive carbon dioxide in the blood), use of accessory muscles for breathing, respiratory acidosis
- Upper airway edema affecting patency of airway
- Neurological impairment: May be secondary to primary illness, encephalopathy, or residual effects of sedation
- Neuromuscular Diseases (Guillain-Barre syndrome, Duchenne Muscular Dystrophy)
- Acute heart failure
- Poor nutrition
- Other risk factors: Severity of illness on admission to ICU, prolonged intubation, continuous sedation

It is essential for the Health Care Provider to identify patients at a higher risk for extubation failure/need for re-intubation, as extubation failure can have detrimental consequences. It is also imperative that all appropriate equipment and personnel are on hand for difficult extubation.
Consequences of Extubation Failure
The incidence of extubation failure has been noted to be between 6% and 47%. Nosocomial pneumonia is significantly increased in patients failing extubation (47% versus 10%). Additional consequences of extubation failure are:
- Prolonged ICU stay and hospitalization
- Prolonged mechanical ventilation
- Need for tracheostomy
- Increased medical cost
- Increased morbidity and mortality
Mortality is increased with increasing duration of time between extubation and reintubation. This is due to deterioration in the patients’ condition leading to organ dysfunction and failure.
Predictors of Extubation Failure
There are many risk factors for extubation failure. It is vital for the Healthcare Provider to do a thorough assessment of extubation readiness. Parameters that are used to predict failure of extubation are often categorized into parameters assessing respiratory mechanics, airway patency and protection of airway, and cardiovascular reserve. Successful extubation is dependent on adequate cough strength, minimal secretions, and mental alertness or the neurological ability to maintain adequate spontaneous breathing.
- Successful spontaneous breathing trials: These trials allow the patient to breath more on their own while the artificial airway remains in place. This allows the Healthcare provider to better assess respiratory muscle reserve/weakness and work of breathing
- Adequate cough strength: Important for patient to be able to clear airway of secretions. This may be affected due to weak respiratory muscles and laryngeal dysfunction
- Secretions: Excessive secretions or the patient’s inability to handle their secretions
- Neurological Dysfunction: Study results vary on the impact of neurological impairment on extubation failure. Most recently, a GCS ≥10 is prerequisite for successful extubation
- Cuff leak: Laryngeal edema and airway obstruction following extubation may lead to extubation failure. When the cuff on the artificial airway is deflated, the amount of leak noted depends on the degree of laryngeal and airway edema. Glucocorticoids (steroids) are often administered prior to extubation to reduce airway edema
- Vital Signs and Blood Gases: Spontaneous breathing requires the heart to work harder. Patients with poor heart function or following cardiac surgery may be at an increased risk for failing extubation. An increase in heart rate and respiratory rate during spontaneous breathing trials may be an indicator of extubation failure. Other findings may include an increase in lactic acid, an increase in PaCO2 (carbon dioxide) in the blood, a decrease in the blood pH (indicating acidosis), or decreased oxygen content in the blood.
Predictors of extubation failure may not apply to neurologically injured patients as the ability to protect their airway and clear secretions may be impaired independently of their ability to ventilate.



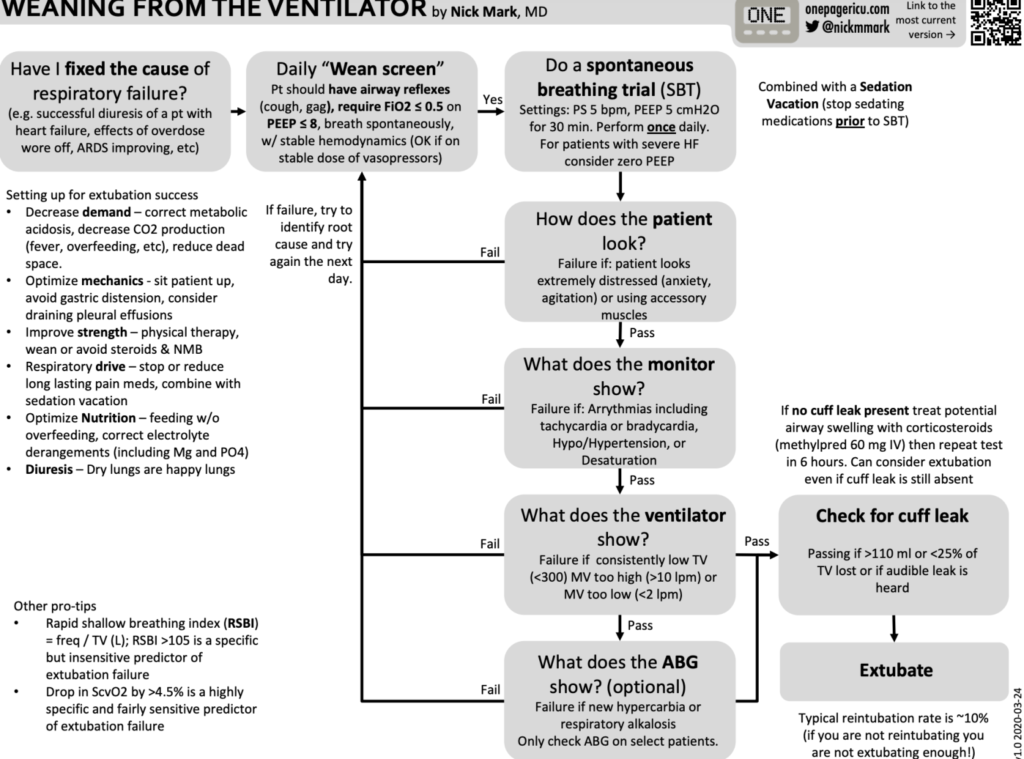
*Photo + caption source: Mark, N. (n.d.). Weaning From The Ventilator Retrieved November 30, 2022, from https://static1.squarespace.com/static/5e6d5df1ff954d5b7b139463/t/5e7a8442e1294b32cd7106b1/1585087555516/ICU_one_pagers_vent_weaning.pdf
Management of Failed Extubation
Extubation failure is a common occurrence in the ICU. Even with successful spontaneous breathing trials, patients remain at risk for extubation failure following removal of the artificial airway due to other factors and circumstances.
- Nasal Intermittent Mandatory Ventilation (NIMV)/Intermittent Mandatory Ventilation (IMV): Use of NIMV/IMV has been shown to provide the additional respiratory support needed to avert/prevent reintubation in some patients.
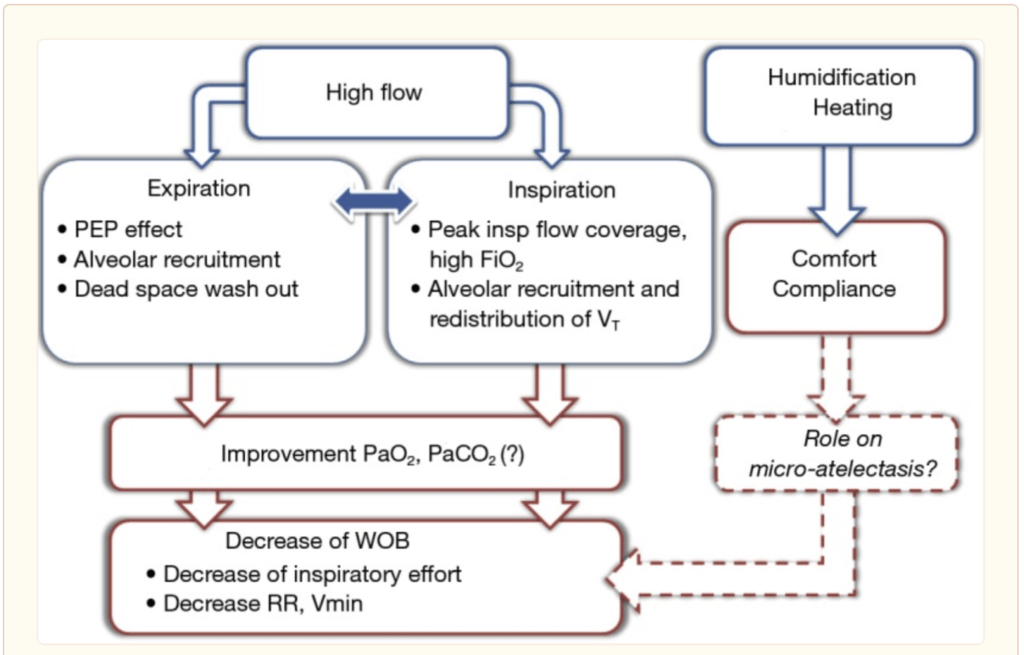
- High-Flow Nasal Cannula: Treatment for hypoxemic acute respiratory failure. Delivers a high flow/fraction of inspired oxygen (FiO2) and generates a low level of positive pressure. This provides support for patients with weak respiratory muscles and improves the work of breathing and respiratory rate.
- Oxygen alone should not be used to correct hypoxemia that is caused by hypoventilation (ineffective breathing and ventilation). In doing so, the respiratory drive can be suppressed and precipitate acute respiratory failure
- Steroids: Edema of the upper airway is difficult to assess before extubation. Upper airway edema is a risk factor for reintubation. Evaluating for a cuff leak prior to extubation predicts stridor but not the need for reintubation. In a double blinded trial, four (20 mg) doses of prophylactic use of methylprednisolone initiated 12 hours before extubation at 4 hour intervals versus placebo, resulted in reduction (22% to 3%) of laryngeal edema and reduction in reintubation (8% to 54%) due to laryngeal edema.
Evidence is suggestive that prophylactic administration of glucocorticoids and early institution of non-invasive ventilation may prevent reintubation in some patients. If necessary, early reintubation and reinstitution of ventilation should be instituted.
References:
Agarwal, A. (2017). Respiratory Care of Patients with Neuromuscular Diseases.
Coplin, W. (2000). Implications of Extubation Delay in Brain-Injured Patients Meeting Standard Weaning Criteria. American Journal of Respiratory Critical Care Medicine, 161, 1530–1536
Frat, J.-P. (2017). High-Flow nasal oxygen therapy and noninvasive ventilation in the management of acute hypoxemic respiratory failure. Annals of Translational Medicine, 5(14).
Kulkarni, A. (2008). Extubation failure in intensive care unit: predictors and management. Indian Journal of Critical Care Medicine, 12(1), 1–9. https://doi.org/10.4103/0972-5229.40942
Kurachek, S. (2003). Extubation failure in pediatric intensive care: A multiple-center study of risk factors and outcomes. Critical Care Medicine, 31(11). https://doi.org/10.1097/01.CCM.0000094228.90557.85




