By Santa J. Bartholomew M.D. FAAP, FCCM
See Corresponding Case Study: Sleep Apnea
Apnea is defined as a pause in the regular breathing pattern during sleep. The causes are many; however, the results are similar in that the interruption of breathing burdens the individual’s respiratory, cardiovascular, and neurological systems. This burden is cumulative over time.
Kinds of Apnea
There are three general kinds of apnea:
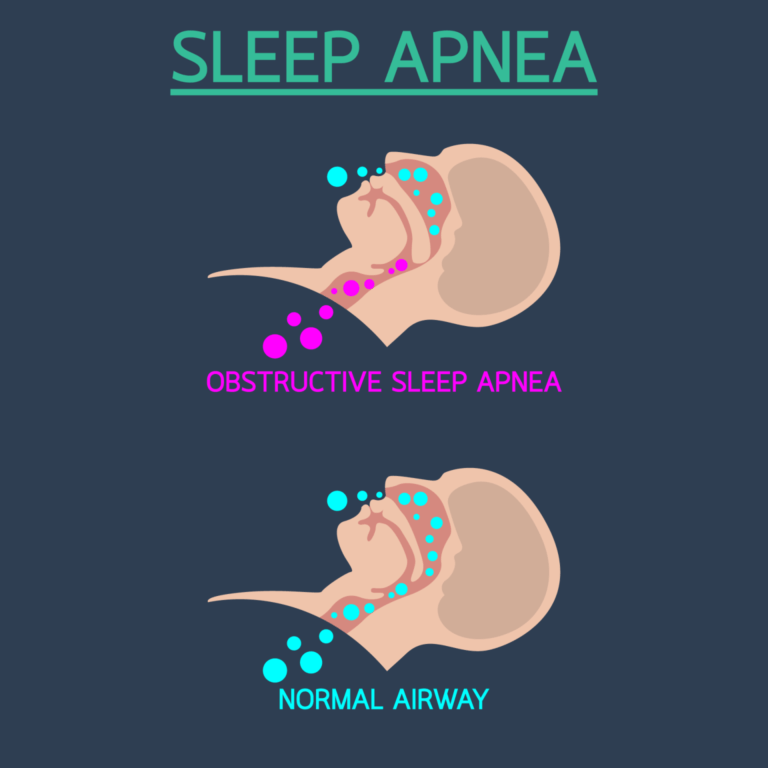
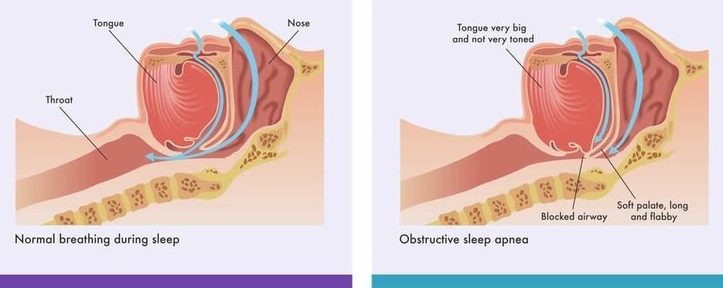
- Obstructive Sleep Apnea is breathing blocked by an “obstruction” of the upper airway while chest and abdominal muscles keep attempting to breathe.
- shallow breathing, snoring with big gasps
- “Central” Sleep Apnea
- breathing takes a pause, the brain “skips a beat”
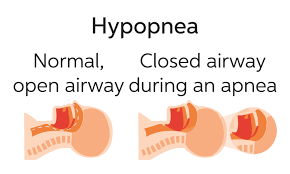
- Hypopnea
- reduction in breathing of about 50%, shallow breath, due to a partially obstructed airway
- small change in oxygen level
- shallow breath
- Rarely requires intervention
Apnea In Children
Pediatric obstructive sleep apnea syndrome (OSAS) is a sleep disorder in which a child’s breathing is partially or entirely blocked repeatedly during sleep. The condition is due to narrowing or blockage of the upper airway. The prevalence of OSAS ranged from 0% to 5.7%, with obesity being an independent risk factor. OSAS can be associated with cardiovascular issues, growth, neurobehavioral abnormalities, and possibly inflammatory changes in the body.
Children with OSAS are most likely to demonstrate behavioral problems unlike their adult counterparts how usually show daytime sleepiness. No matter how OSAS is revealed in adults and children it may residual complications if not treated.
The most common underlying condition in children is the enlargement of the adenoids and tonsils. Therefore, the primary treatment is typically adenotonsillectomy (AT). Usually, this results in significant improvements in behavior and attention and can also improve cognitive abilities. Although OSAS will often improve postoperatively, children may have residual problems, especially if they are in the “obese” category on the BMI scale.
Following an adenotonsillectomy (AT), if residual obstruction remains, is one common therapy used to treat the issue:
- CPAP (continuous positive airway pressure): a machine that delivers a steady stream of air. The airstream pushes against any obstructions, maintaining an open airway for breathing. CPAP machines are used to treat OSAS.
- Though respiratory therapy may be effective in treating OSAS, adherence is a significant barrier for children. For this reason, CPAP is not recommended as first-line therapy for OSAS when AT is an option.
- Though respiratory therapy may be effective in treating OSAS, adherence is a significant barrier for children. For this reason, CPAP is not recommended as first-line therapy for OSAS when AT is an option.
Children with Down syndrome are most vulnerable to obstructive sleep apnea because of their unique craniofacial anatomy and hypotonia (poor muscle tone).
- Smaller mid-face: typically, people with Down syndrome have a smaller upper jaw, and/or nose.
- A smaller jaw makes the tongue seem larger and this can cause an obstruction.
- Decreased pharyngeal muscle tone: pharyngeal muscles are the muscles that support breathing, and those muscles can be weaker in people with DS.
Timely recognition and treatment of OSA in this population of children is an important to achieve optimal cognitive function and quality of life. Although guidelines recommend routine OSA screening in young children with Down syndrome, it can be difficult to perform, and the results are often uncertain.
The National Down Syndrome Society (NDSS) promotes awareness of OSA for individuals with Down Syndrome. Their website states: “There is a 50-100% incidence of obstructive sleep apnea in individuals with Down syndrome, with almost 60% of children with Down syndrome having abnormal sleep studies by age 3.5 -4 years.”
In 2011, the American Academy of Pediatrics recommended that all children with Down syndrome have polysomnography, or a sleep study, by four years of age. The sleep study consists of a night of observed sleep during which professionals measure brain waves, the oxygen level in the blood, heart rate, breathing, and eye and leg movement. Children who cannot have a sleep study PSG due to lack of access or inability to tolerate the conditions may have a home sleep study or pulse oximetry as an initial screening.
CPAP and BiPAP machines are typically life-long treatments. Although many individuals with Down syndrome adjust to using the CPAP during sleep, some cannot tolerate wearing the facial mask and require alternative therapies.
Research suggests that OSAS is also a risk factor other diseases:
- Reactive airways with bronchoconstriction
- Research confirms that asthmatic patients are more prone to develop OSAS symptoms than people who do not have asthma
- Nasal obstruction due to allergies is one of the characteristics of asthmatics that increase OSAS symptoms and increase the collapse of the upper airways
- Gastroesophageal reflux
- Generalized inflammation of airways
- OSAS-induced cardiac dysfunction have been proposed as factors that worsen asthma control.

Neonatal apnea is a condition that affects both term and pre-term infants for various reasons, though it is more common in preterm infants. Unlike periodic neonatal breathing that combines a regular respiratory pattern and respiratory pauses, neonatal apnea and apnea of prematurity are defined as the absence of breathing for more than 20 seconds.
Clinical manifestations of neonatal apnea require careful management, including invasive or noninvasive treatment, ventilation, monitoring, and pharmacology intervention to prevent acute and long-term complications. When a neonate, preterm or not, has a classic apneic event, they will cease breathing for 15-20 seconds and have no respiratory effort. This may be accompanied by bradycardia and some oxygen desaturation; the baby will also bluish tint to the skin.
This is one of the more common conditions diagnosed in the neonatal intensive care unit. Apnea is caused by immaturity of the neurological system and weakness of the muscles that keep the airway open. At times, additional stresses, specifically in a premature baby — including infection, heart or lung problems, low blood count, low oxygen levels, temperature problems, feeding problems, and overstimulation, may cause or enhance incidents of apnea. Recurrent apnea can lead to respiratory failure, pulmonary hemorrhage, abnormal heart and lung function, intracranial hemorrhage, abnormal nervous system development, and even sudden death.
Caffeine citrate has been used for treating apnea since 1970 due to it’s excellent bioavailability and paucity of side effects. Varying doses of caffeine citrate for apnea have been proposed. The safe and effective amount of low and high caffeine citrate maintenance doses for apnea treatment of premature infants has been determined by analysis of multiple clinical studies. Higher-maintenance doses of caffeine citrate appear more effective than low-maintenance doses for the treatment of apnea despite a high incidence of tachycardia.
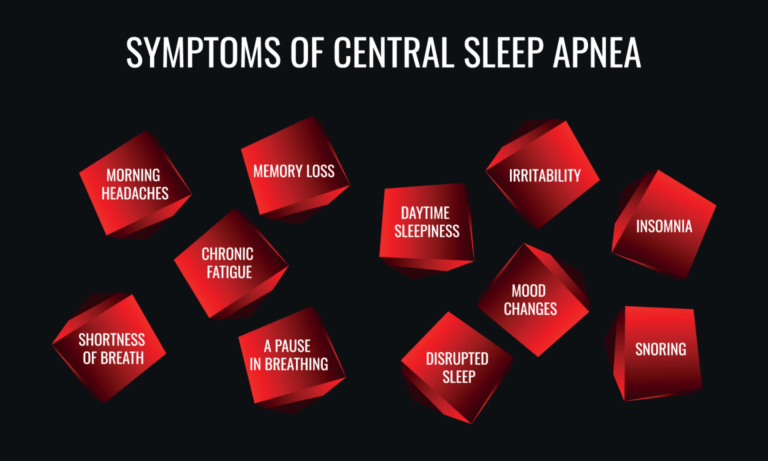
Central sleep apnea (CSA) is less common than neonatal or obstructive sleep apnea. It is a pause in breathing during sleep, usually without snoring or gasping. Everyone experiences central apneas occasionally. However, if it occurs too frequently or for long periods, it can cause a decrease in the oxygen levels in the body, disrupt sleep and impact neurologic development in children.
Central sleep apnea is caused by increased sensitivity to the partial pressure of CO2 in the system that regulates the respiratory drive. CSA commonly presents as cycles of deep, rapid, crescendo decrescendo breathing (hyperpnea), followed by slower, shallower breathing (hypopnea) or no breathing without respiratory effort from the diaphragm (apnea), known as Cheyne-Stokes breathing.
The cause of CSA in children is either idiopathic or due to a profound neurological insult at birth or after. CSA can lead to systemic and pulmonary hypertension, arrhythmias, and cardiovascular collapse is untreated.
Characteristics of central sleep apnea include:
- Observed episodes of pauses in breathing or abnormal breathing patterns during sleep
- Abrupt awakenings followed by shortness of breath
- Frequent awakenings in general
- Headaches in the morning
- Difficulty focusing and concentrating
- Daytime sleepiness (if sleep is disturbed)

BiPAP machines offer three air-pressure settings which include spontaneous switching that senses breathing patterns and adjusts accordingly, timed switching which is better for those who need a regular rate and spontaneous timed switching that is a mix of both. BiPAP is better for those with central sleep apnea since they assist with air trapping and can provide a backup respiratory rate when the patients has to long a period of apnea.
References:
Abu-Shaweesh JM, Martin RJ. (2005) Apnea of prematurity: past, present, and future. J Arab Neonatal Forum; 2:63-73.
Chen, J; Chen, X (2008) BioMed Research International, (8)1-11.
Deakins, K (2011) Management of Neonatal Apnea, AARC Times, 35(11): 5-8.
Hill CM, Evans HJ, Elphick H, et al. (2016) Sleep Med (27)28: 99–106
Javaheri S, Dempsey JA. (2013) Central sleep apnea. Comprehensive Physiology. (3): 141‐163.
Alkhalil, M, Schulman, E, Getsy,J, 2009 Obstructive Sleep Apnea Syndrome (OSAS) and Asthma: What are the links? J Clin Sleep Med. 5(1): 71–78.
Sleep & Down Syndrome | National Down Syndrome Society (NDSS)




