By Santa J. Bartholomew M.D. FAAP, FCCM
The category of inflammatory bowel disease (IBD) is divided into two specific categories: Crohn’s disease and Ulcerative colitis, both of which are diagnosed in late childhood or early adulthood. IBD is one of the major chronic gastrointestinal diseases among children and adolescents in the westernized world.
- Both are characterized by a chronic and debilitating condition defined by a relapsing episode of GI inflammation. In Ulcerative colitis (UC), this includes the superficial lining of the bowel starting at the rectum, and it is limited to the colon. In Crohn’s disease (CD), the inflammation can affect any part of the GI tract from mouth to colon, and it is transmural (across the entire bowel wall).
- Pediatric patients often have more severe disease of both UC and CD than their adult counterparts.
- In children, there is a male predominance
- 25% of IBD occurs in childhood, the rest in early adulthood, with the worst of the disease peaking in the second and third decades of life.
- Incidence: Crohn’s Disease: 40/100,000 and Ulcerative Colitis
- Approximately 1.4 million people suffer from IBD in the USA
- A subset of children acquire IBD at a very early age and this is thought to be a different type of IBD than what is seen in older children.
What Is the Cause of IBD?
The cause of IBD is unknown, but there are several theories:
- Dysregulation of the hosts immune system to the normal bacteria that live in the bowel
- Genetic component
- Alterations in the bacterial biome of the gut
- Environmental exposures- since IBD is a Western world disease, it seems reasonable that our diet and food hygiene may play a role in the development of IBD.
Symptoms of IBD
Presenting symptoms: can be HIGHLY VARIABLE.
- Abdominal pain: varying quality and location.
- Nausea and vomiting
- Rectal bleeding
- Diarrhea
- Weight loss
- Growth delay
Pediatric patients often have more severe disease of both UC and CD than their adult counterparts.
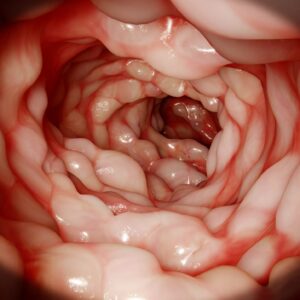
Crohn’s Disease
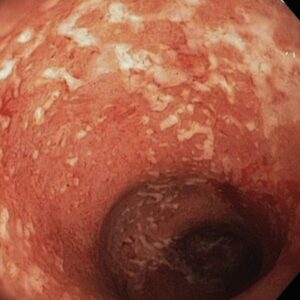
Ulcerative Cholitis
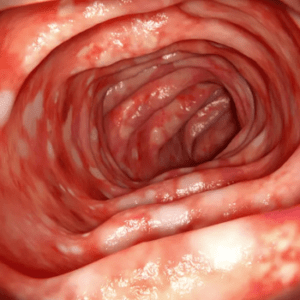
Inflammatory Bowel Disease
Diagnosis
Differential Diagnosis Considerations With Inflammatory Bowel Disease
More Likely to Present with Chronic Complaints
- Growth failure
- Irritable Bowel syndrome
- Lactose intolerance
- Ovarian cyst
- Celiac disease
- Acid-peptic disease
- Anorexia nervosa
- Excess laxative intake
- Lymphoma
- Constipation
- Sorbitol Ingestion
Peds in Review:37(8) Aug 2018
More Likely to Present More Acutely
- Appendicitis
- Mesenteric adenitis
- Fissure-in-ano
- Hemorrhoids
- Colonic polyps
- Meckel diverticulum
- Acute infections
- Clostridium dificile,
- Salmonella/Shingella/Compylobacter species
- Yersinia species
- Giargia species
- Entamoeba histolytica
- Parasitic infections
Laboratory Data: 20% of children have COMPLETELY NORMAL LABS
- There is no test specific for IBD, but in most of these children, inflammatory markers like CPR, and ESR are elevated
- Albumin can be low because of poor nutritional health
- Chronic inflammation of the bowel can lead to malabsorption, so vitamin and Zinc levels may be low
- There can be other organs affected, such as the liver, and then one would see elevated transaminases
Other organs affected:
Comorbid Signs and Symptoms of Inflammatory Bowel Disease by Organ System
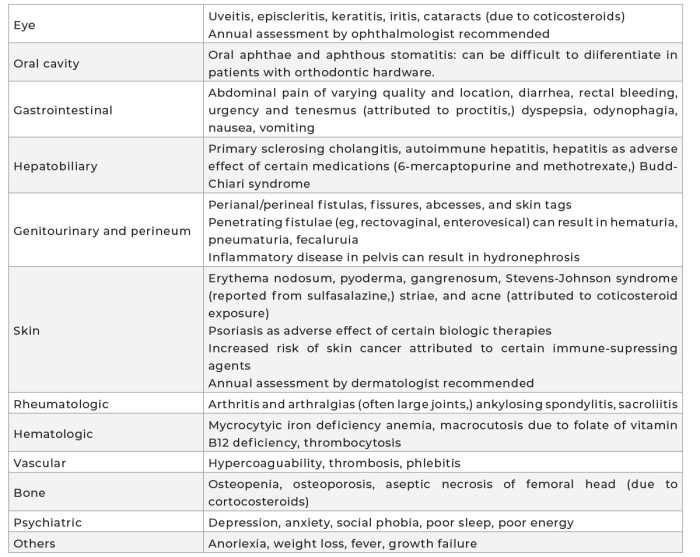
Peds in Review:37(8) Aug 2018
Diagnosis:
- Children suspected of IBD need a referral to a GI specialist
- Endoscopic examination and biopsies help confirm the diagnosis and determine UC from CD
- One-third of patients cannot be classified into either category as there is inflammation of the ileum.
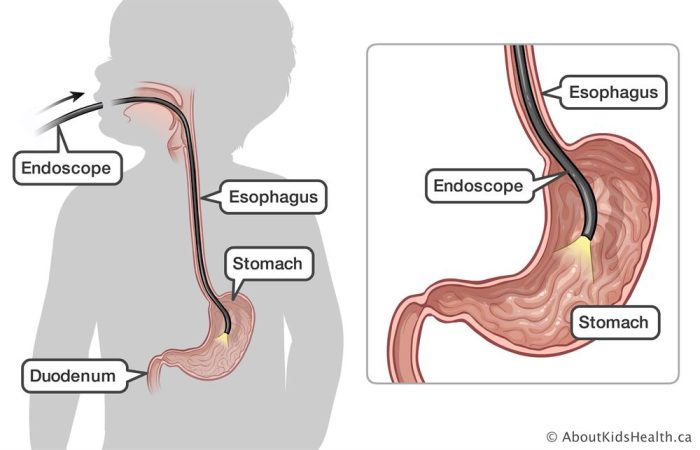
During an upper endoscopy, a thin flexible tube with a camera on the end is inserted into the mouth and down the esophagus to look at the esophagus, stomach, and duodenum.
Treatment for IBD
Treatment involves controlling active symptoms and trying to prevent long-term complications. Treatment, however, is complicated as many of the therapies can impact the growth of the child.
- STEROIDS: help induce remission in both UC and CD, but fewer than a third of patients achieve true healing of the bowel mucosa so it can go back to normal function
- ENTERAL NUTRITION: giving 100% of the nutritional needs of the child as a liquid diet is also used to induce remission and help heal the mucosa
- AMINOSALICYLATES: are topical anti-inflammatory drugs that help decrease inflammation in the bowel, such as Sulfasalazine
- IMMUNOMODULATORS: Also assist in attaining and maintaining remission but come with significant side effects such as myelosuppression, chemical hepatitis, pancreatitis, and in a small number of cases lymphoma
- ANTI-TNF THERAPY: biologics such as Infliximab, Adalimumab, and Golimumaub that are used to induce remission in children resistant to steroids or who are steroid dependent despite using an immunomodulator. The can, however, cause a psoriasis-like rash, and increased risk of infection, particularly fungal, viral, and mycobacterial infections
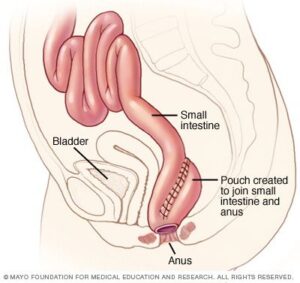
- SURGERY: total colectomy with an ileal pouch is used in children refractory to medical therapy
Long-term problems:
- Growth failure in 40% with CD and 10% with UC
- Vitamin deficiencies: Iron, Folate, Vitamin B12, and Vitamin D
- Colon cancer
- Depression and anxiety disorders
References:
Rosen, et.al Inflammatory Bowel Disease in Children and Adolescents JAMA Pediatr 2015 Nov; 169(11):1053-1060.
Sauer Cary, Kugathasan Subra. Pediatric Inflammatory Bowel Disease: Highlighting Pediatric Differences in IBD. Gastroenterol Clin N Am 38(2009)611-628.
Shapiro, Jason, Subedi Shova, LeLeiko Neal. Inflammatory Bowel Disease. Peds in Rev 37(8)337-347.
Levine A.,et.al. ESPGHAN Revised Porto Criteria for the Diagnosis of Inflammatory Bowel Disease in Children and Adolescents. JPGN 58(6):795-806.




