By Santa J. Bartholomew M.D. FAAP, FCCM
Acute pancreatitis is one of the leading gastrointestinal causes of hospitalizations in the United States, and is increasingly being diagnosed in children within the past two decades.
Characterized by an acute inflammation of the pancreas, older children often present with a sudden onset of persistent, severe mid-abdominal pain that may radiate to the back. Younger children and infants may present with more generalized abdominal discomfort, irritability and vomiting.
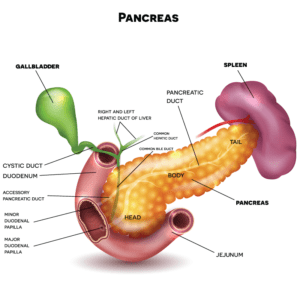
The Pancreas
The pancreas is in the abdomen just behind the stomach. The pancreas makes enzymes during digestion that break down sugars, fats and starches. Hormones produced in the pancreas help the digestive system.
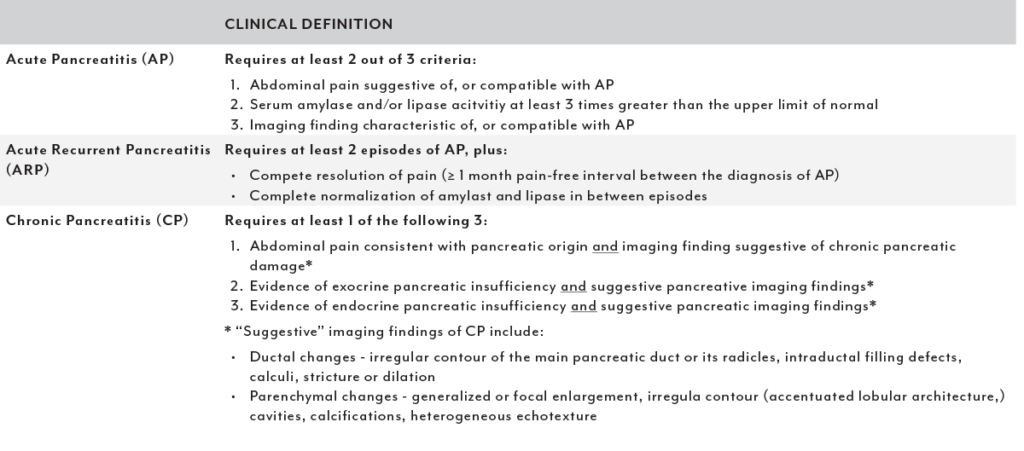
Classification
Pancreatitis in children may be mild, moderate, or severe. More severe episodes of pancreatitis typically have more complications. Acute pancreatitis may progress to acute recurring pancreatitis (ARP) or chronic pancreatitis (CP).
Table 1: Definitions of Pancreatitis in Children (Insppire Criteria)
Etiology
- Genetic: <10% in acute pancreatitis, >50% in reoccurring pancreatitis, ~75% in chronic pancreatitis
- Anomalies of the pancreas: ~ 5-20% of children with acute pancreatitis
- Gallstones: most common cause in children. 3-30% of cases
- Medications: contribute up to one-fourth of cases
- Trauma: accidents and non-accidental trauma from child abuse
- Metabolic Disorders: high calcium levels most common in children. Inborn errors of metabolism
- Infection: mumps, herpes, salmonella
- Other illness: Lupus, Kawasaki disease, inflammatory bowel disease
Diagnosis
Acute pancreatitis is diagnosed based on the patient’s history, physical exam, and supported by laboratory tests and imaging as indicated. Physical findings on exam will vary based on the severity of disease.
Diagnosis requires two of the following three criteria:
- Sudden onset of severe mid-abdominal pain that does not go away. This pain may radiate to the back.
- Increase in enzymes made by the pancreas more than three times their normal level
- Findings specific to pancreatitis on an ultrasound of the stomach, computed tomography (CT) of the stomach or magnetic resonance imaging (MRI) of the stomach
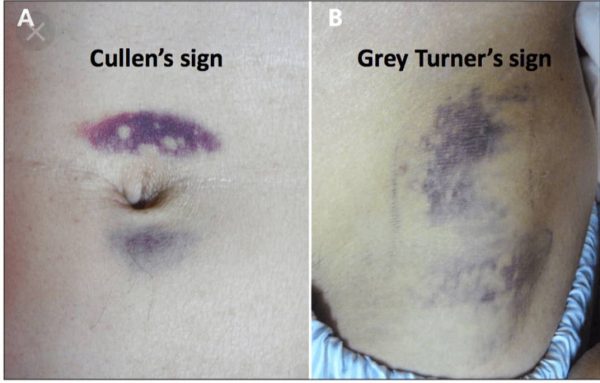
Classic Examination Findings
- Tenderness to mid-abdomen, abdominal distention, yellowing of the eyes, fever
- 3% of patients with acute pancreatitis may have a bluish discoloration around their umbilicus (Cullen’s sign) or a bluish discoloration along their flank (Grey Turner’s Sign)
- Some patients may experience:
- Shortness of breath because the diaphragm just above the pancreas gets inflamed and this may progress to acute respiratory failure.
- 5% of children have hemodynamic instability and end organ failure such as renal failure and shock.
Differential Diagnosis of Pancreatitis
- Peptic Ulcer Disease (PUD)
- Gallstones
- Cholecystitis
- Perforated viscus
- Intestinal obstruction
- Mesenteric Ischemia
- Hepatitis
Acute pancreatitis is diagnosed based on the patient’s history, physical exam, and supported by laboratory tests and imaging as indicated.
Laboratory Signs
- Elevated amylase and lipase: these are enzymes secreted by the pancreas.
- Lipase: elevations are highly sensitive for pancreatitis (85-100%) and rise within 4-6 hours of the onset of symptoms and generally return to normal within 8 to 14 days
- Amylase: elevations with 6 to 12 hours but usually returns to normal within 3-5 days. Serum amylase > three times upper limit of normal has 67 to 83% sensitivity for acute pancreatitis.
- The “gold standard” for diagnosis of acute pancreatitis: elevated lipase and amylase
- Markers of immune activation:
- Increase C-reactive protein
- Increase procalcitonin.
- Increase TNF
- Elevated white count
- Signs of third spacing
- Elevated hematocrit from hemoconcentration
- Elevated BUN and creatinine
- Hyperglycemia/hypoglycemia: with broad swings in insulin levels- insulin also being a hormone secreted by pancreas.
Imaging
- X-ray of abdomen may show distention of bowel/intestines
- Abdominal Ultrasound- First choice of imaging in pediatrics
- Abdominal CT- is not needed to diagnose pancreatitis
- Magnetic resonance cholangiopancreatography (MRCP) – a special kind of MRI used to look at the pancreas and the organs around the pancreas. Is quickly becoming study of choice in pediatrics
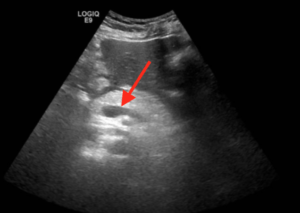
Ultrasound of a Human Pancreas
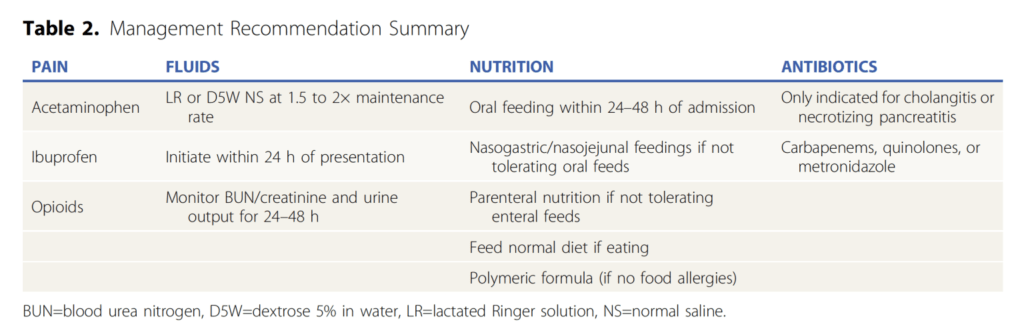
Management and Treatment
- Supportive care with fluids, pain control, and nutrition.
- Change in therapy in recent years has been towards feeding through the acute phase of pancreatitis.
- If unable to take fluids and medications by mouth, may require hospitalization for IV fluids and nutrition through a feeding tube or an IV.
- Treat any underlying diseases or predisposing factors for pancreatitis.
- If there is an obstruction to flow of secretions from pancreas, then ERCP (endoscopic retrograde cholangiopancreatography) may be needed. While it is not as commonly used in children as in adults has become an invaluable tool in helping treat obstruction.
- Islet auto-transplantation (TPIAT) has become the surgery of choice for recurring pancreatitis and chronic pancreatitis. This entails all or part of the pancreas is removed, and special insulin producing cells being placed in the liver as an alternative.
Nguyen,T. (N.D.). Pancreatitis [Review of Pancreatitis]. 41(10).
Complications and Prognosis
Most children presenting with acute pancreatitis will have mild pancreatitis. Complications that may occur from pancreatitis range from mild to more severe including:
- Infection
- Fluid collection around the pancreas
- Pancreatic Pseudocyst: encapsulated collection of necrotic tissue, secretions or blood
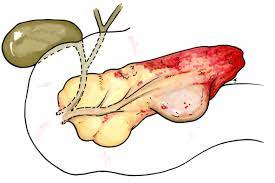
- Pancreatic Necrosis: an area of tissue in the pancreas dies due to too little blood supply
The mortality rate for acute pancreatitis in children is <5%. In ~ 15-35%, their pancreatitis will reoccur. Children with acute reoccurring pancreatitis and chronic pancreatitis tend to have more genetic and/or anatomical risk factors compared to adults who tend to have more environmental risk factors. In adolescents, autoimmune and environmental risk factors begin to emerge.
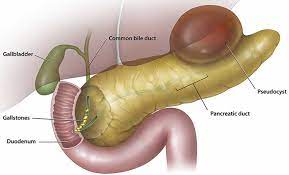
Pancreatic Pseudocyst
Pancreatic Necrosis
References:
Nguyen,T. (n.d.). Pancreatitis [Review of Pancreatitis]. 41(10).
Pancreatitis in Children: Short Title: Pediatric Pancreatitis. Aliye Uc, MD
Up-to Date: 2022: Clinical manifestations and diagnosis of acute pancreatitis
Up-to Date: 2022: Etiology of acute pancreatitis
Up-to Date: 2022: Management of acute pancreatitis




