By Santa J. Bartholomew M.D. FAAP, FCCM
Heat Stroke in Children
Heat illnesses represent one of the most hazardous conditions for our young athletes, children, and other vulnerable populations during the summer months in the United States. Heat stroke is the worst of heat illnesses along a spectrum and is characterized by temperature >104.9, central nervous system dysfunction (altered mental status, seizures, coma) and multi-organ failure.
Heat Stroke is classified into two specific categories, exertional and classic.
Exertional Heat Stroke
Exertional Heat Stroke is related to strenuous activity in heat: football practice in August before school starts, firefighters, laborers, and soldiers in the extreme temperatures. Heat Stroke can occur with as little as 60 minutes of extreme activity and is typically triggered by strenuous activity in high ambient temperature and humidity. This time frame can be altered by using alcohol and illicit drugs (amphetamines, cocaine, LSD and methamphetamine) that may alter ability to sweat and dissipate heat or cause further rise in core temperature.
Surveys reveal a steady rise in morbidity and mortality in high school football players and army personnel from exertional heat stroke in the last decade.
Epidemiology
- Surveys in the USA reveal a steady rise in morbidity and mortality in high school football players and army personnel from exertional heat stroke in the last decade.
- 702 deaths in children annually from 2004
- Third major cause of death in teens behind trauma and cardiac death

Pathophysiology
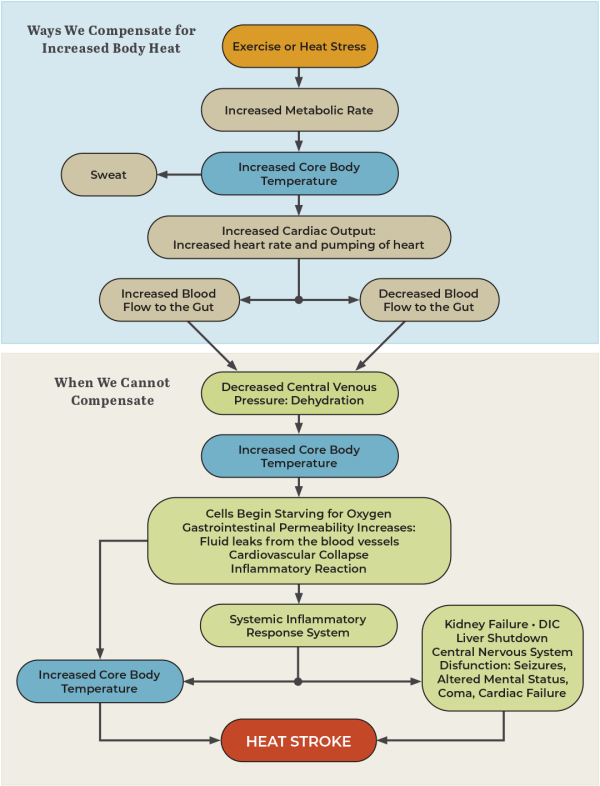
- HS occurs when evaporation (our major way of disposing of heat) cannot occur such as in high temperature and humidity.
- HS occurs when cardiac output is insufficient to deal with the very high thermoregulatory needs of the person. So, athletes that are no hydrated properly for the heat and humidity and without cool down breaks in between practice exercises.
- Core temperature rises
- Cells in body organs begin to die setting off an inflammatory cascade causing injury to the tissues of all the major organs.
- Prolonged heat exposure leads to collapse of blood pressure, fluid pouring into the lungs causing low oxygen and suffocation and ultimately shut down of organs and death.
- Children present with temperatures 104°F to 105°F (core temperature.)
- CNS symptoms that can be very subtle such as impaired judgement or inappropriate behavior (sometimes misdiagnosed when alcohol or illicit drugs are involved), seizures, hallucinations, gait disturbances, seizures, com.
- Children are usually very tachycardic and tachypneic
- Skin is warm, may be sweaty and flushed
- Vomiting and diarrhea common- sometimes bloody vomiting and diarrhea
- May have large areas of purpura (purple bruises on their skin)
Lab findings: include evidence of clotting problems, liver and kidney dysfunction, high potassium levels, high or low sodium levels and high CPK (an enzyme found in the blood with muscle breakdown).
Treatment:
- Pre-hospital:
- Cold-water immersion (most effective treatment for adolescents) or tarp assisted cooling.
- Removal from the heat source (the key is rapid cooling) as soon as possible to diminish the risk of morbidity and mortality.
- Administration of room temperature IV fluids.
- In Hospital:
- Continue rapid cooling
- Airway management depending on circumstances. Some children will be wakeful and able to protect airway and others will need intubation.
- Fluid resuscitation to replenish lost fluid this will most likely be 40 to 80 mls/kg of isotonic fluid.
- Treatment of shock and support of the heart and blood pressure.
- May continue rapid cooling with addition of ice bags to neck, axilla and groin. Avoid Shivering which Increases Body Temperature.
- May need to use benzodiazepines to suppress shivering.
- Treatment of injury to end organs.
- Treatments that are Ineffective:
- Tylenol and Ibuprofen do not treat hyperthermia and may be damaging the liver, kidneys and stomach of these children.
- Alcohol baths can be absorbed by the skin and lead to toxicity.
- Dantrolene used for malignant hyperthermia associated with anesthesia has not been shown to have consistent benefit
- Mortality: 1% to 15% in adolescents and young adults.
- Permanent neurologic damage is more common especially if initial temperature is 107.6°C or higher.
Classic Heat Stroke
Classic Heat Stroke usually occurs in epidemic fashion in the elderly and other vulnerable populations that cannot physiologically adjust to the stress of high ambient temperatures. According to the US Weather Service heat waves kill more people than any other weather event.
Prepubertal children are at risk for classic heat stroke
- They have a high ratio of surface area to body mass leading to increased heat absorption. They have poorly developed thermoregulation that impairs their ability to dissipate heat.
- Small blood volume relative to body size limiting the potential for heat conductance and causing a greater accumulation of heat in the body
- Low sweating rate reducing the potential for heat dissipation through sweating
- In infants and small children, they are further at risk because they are immobile and when left in very hot environments death occurs within a few hours.
Characteristics of Classic Heat Stroke
- Sweating absent
- CNS dysfunction is common
- Renal failure uncommon
- Labs usually normal
- Patients are usually prepubertal or elderly and chronically ill
Clinical presentation
- Elevated core body temperature
- Weakness, lethargy, nausea and dizziness
- Flushing
- Non-cardiac pulmonary edema
Treatment
- Airway management depending on circumstances. Some children will be wakeful and able to protect airway and others will need intubation.
- Fluid resuscitation to replenish lost fluid this will most likely be 40 to 80 mls/kg of isotonic fluid.
- Treatment of shock and support of the heart and blood pressure.
- May continue rapid cooling with addition of ice bags to neck, axilla and groin. Avoid shivering which increases body temperature.
- May need to use benzodiazepines to suppress shivering.
- Treatment of injury to end organs
Prognosis
- Patients with classic heat stroke are often elderly with many comorbidities mortality is upwards of 60%.

References:
Abderrezak B, et.al. Heat Stroke NEJM 346:25. June 2002 pp 1978-1988.
Casa Douglas. Exercise in the Heat Part II: Critical Concepts in Rehydration, Exertional Heat Illness and Maximizing Athletic Performance. J Ath Training 199;34(3):253-262.
Coris,Eric, Ramirez Arnold, Van Durme Daniel. Heat Illness in Athletes: The Dangerous Combination of Heat, Humidity and Exercise. Sports Med 2004;34(1); 1-8.
Kenny Glen P.,et.al. Heat Exhaustion. Handbook of Clinical Neurology. Vol157(3) Chapter 31; pp505-530.
Ishimine Paul. Heat Stroke in Children Up-to-Date.




